They're tasked with helping us get better when we're sick, but what about the health and wellbeing of doctors themselves?
Author Lucy Mayes was prompted to look at the pressures doctors are under when her own physician husband, Richard, was nearing burnout.
She's written a book called Beyond the Stethoscope: Doctors' Stories of Reclaiming Hope, Heart and Healing in Medicine, which includes interviews and insights with a number of doctors on both sides of the Tasman.
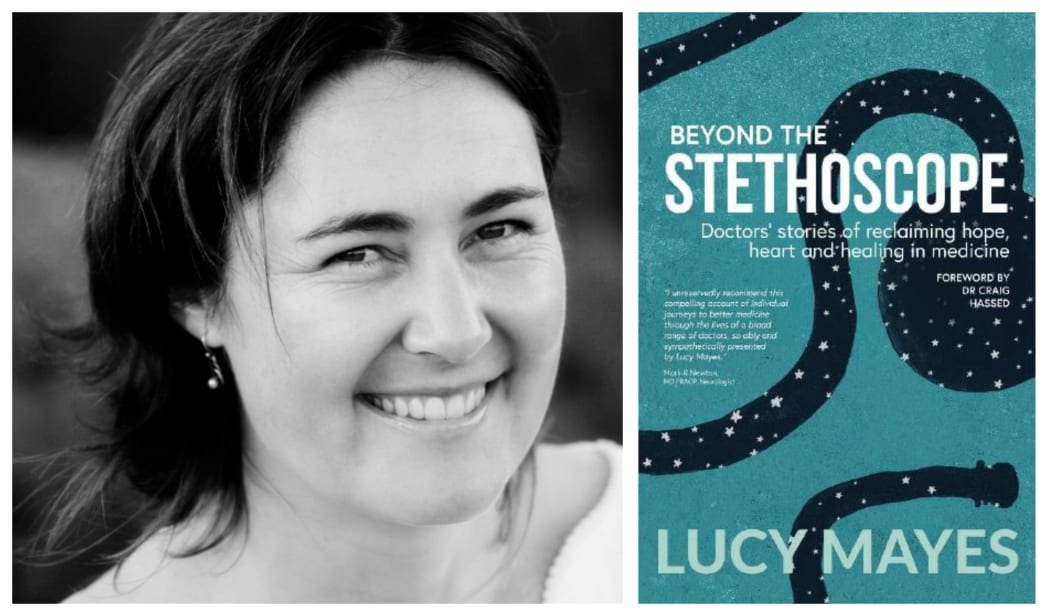
Photo: Supplied
Lucy says her husband Richard’s burnout got so bad that the couple had to move away from the small community they were living in “…he’d got himself into a situation where he was on-call 24/7 and trying to be all things to all people”.
Despite the move Lucy watched her husband still struggle with the conditions of working and trying to reclaim his health and wellbeing. When she read some of his medical magazines she realised burnout and suicidality in doctors is at terrifying rates, she was worried he would become one of these statistics.
When Richard came home and told he he no longer was happy with seeing patients for only ten minutes at a time, Lucy told him it would be a tragedy if he left the profession, and that she would go and find others like him who listen deeply, care deeply and think about the whole human not just their cones and biochemistry.
“Initially is was a journey to demonstrate to Richard that he wasn’t alone in the way that he wanted to practise medicine and had an instinct around what quality health and wellbeing looked like for both himself and his patients. Eventually it really became a passion that was separate from him and our marriage and I realised that this was a much bigger story that needed to be told and perhaps I was the one to do the telling.”
Lucy didn’t struggle to find doctors who were struggling.
She says in New Zealand 75 percent of female doctors and 50 percent of male doctors are struggling with burnout.
“That is extraordinary, it’s really a crisis that needs to be addressed.”
Lucy says people she spoke to who work in hospitals told her that there is a real stigma and shame attached to mental health issues and as a result they keep them very private.
It’s the cultures and attitudes of traditional medicine that aren’t equipped to deal with the crisis, she says.
A number of doctors withdrew their stories after being interviewed for the book because of how difficult it is to have it out their voice in the world, says Lucy, even Richard himself struggled, not wanting to become a poster boy.
Richard says it’s hard to be vulnerable and to share his story but says Lucy was great at holding space for this to happen.
“What I discovered through Lucy’s ongoing encouragement was it’s this vulnerability that creates change.”
He says there’s one particular example when he really felt medicine is going down the route of being a quick fix. When a patient, who was post-menopausal and on HRT and anti-depression medication, came in for cholesterol problems he realised that these short appointments were not so much about finding preventative measures or looking at how the bigger picture, but about medicating people for their symptoms.
“That was frustrating me because I didn’t feel like I was making a difference in people’s lives, they were coming to get well and we were just putting out fires and not stopping the spark.”
Lucy says burnout is a very complex issue, with lots of contributing factors. Among them is the fact that people attracted to medicine are A-type personalities, with perfectionist tendencies. These are people who have a fear of failure and beat themselves up if they get anything wrong, she says, and a lack of sleep and fatigue come into play.
These things in the medical profession can have deadly consequences, she says.

