When she imagines the future of cancer treatment, Yasmin Nouri sees a very different landscape. Instead of chemotherapy, a blunt technique aimed at all fast growing cells, she envisions therapies that are personalised to the patient and targeted towards cancer cells.
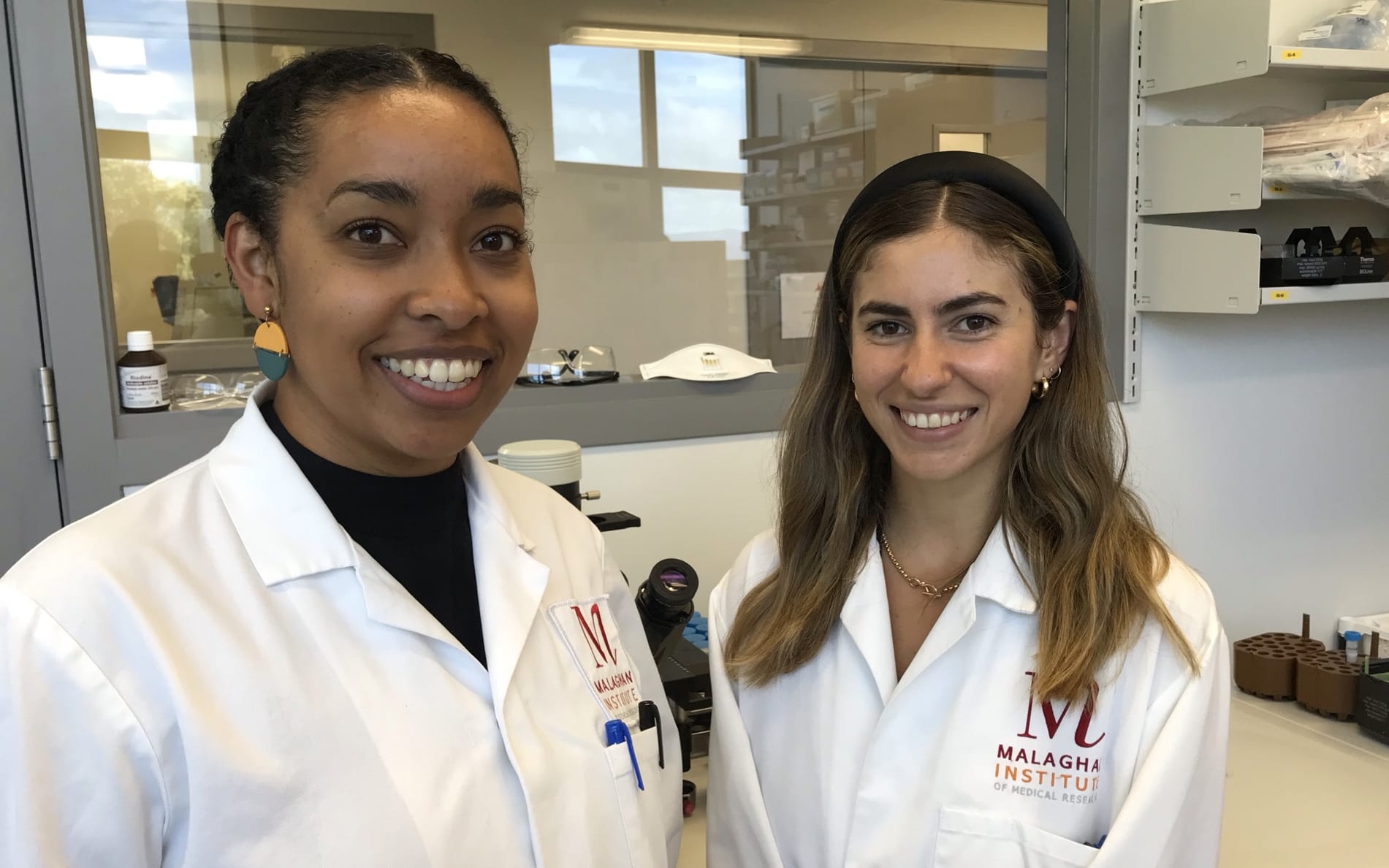
Dr. Patricia Rubio-Reyes and Yasmin Nouri Photo: RNZ / Claire Concannon
Follow Our Changing World on Apple Podcasts, Spotify, Stitcher, iHeartRADIO, Google Podcasts, RadioPublic or wherever you listen to your podcasts.
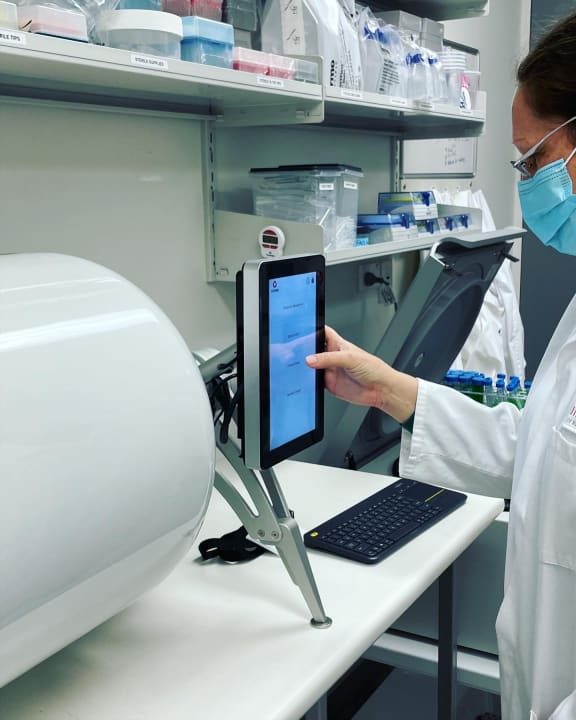
The new Cocoon equipment that will make CAR T-cells. Photo: Supplied / Malaghan Institute for Medical Research
Yasmin hopes that she can play a part in the development of this next phase of cancer therapies. In her final year of her PhD at the Malaghan Institute for Medical Research, she is researching a type of cancer treatment called CAR T-cell therapy. In this therapy, the patient’s own immune cells, their T-cells, are genetically modified so that they have a new receptor on them – one that recognises cancer.
Normally our T-cells don’t recognise cancer cells as an issue because they are our own cells, rather than a virus or bacteria. The added Chimeric Antigen Receptor (CAR) allows the T-cells to do their job, which is to target and kill threats to the body.
In particular, Yasmin is working alongside the Phase I clinical trial currently underway to investigate the safety and efficacy of the CAR T-cell therapy that has been developed at the institute. This trial is specific to patients with a certain type of B-cell lymphoma who have exhausted all other treatment options. Yasmin is running tests in the lab to get into the nitty-gritty of exactly how this therapy works in the body.
She is part of the CAR T-cell therapy research team led by Dr. Rachel Perret. Some CAR T-cell therapies are currently licensed for use in other countries, including the US, the UK and Australia. However, they are expensive, can have serious side effects, and can only be used on particular types of cancers. The aim of the research team is to investigate ways to make CAR T-cell therapy safer, more effective, cheaper and applicable to a wider range of cancers.
Also part of the team is postdoctoral fellow Dr. Patricia Rubio-Reyes. Patricia is focused on research to make CAR T-cell therapy safer, by installing an ‘off’ switch that will kill off the T-cells if side effects occur. She is also investigating how CAR T-cells could be used to target cancers that cause tumors.
Listen to the episode to hear Rachel, Yasmin and Patricia discuss their research and their hopes for the future of cancer treatment.

Dr. Rachel Perret leads the CAR T-cell immunotherapy research team at the Malaghan Institute. Photo: Supplied / Malaghan Institute for Medical Research
To learn more:
- Visit the Malaghan Insitute’s website to read an article about Patricia, learn more about the trial and about scaling up using the new cocoon equipment.
- Listen to this episode where the K9 Medical Detection team discuss their work using dogs to identify prostate and bowel cancers.
- In this episode Brian Cox of the University of Otago talks about studying the causes of cancer.

